TAX TIPS
(1) If a person needs a personal aide because of a medical condition (dementia is a medical condition), the cost of the aide may be a medical expense. (2) If you pay for more than 50% of a person's needs, and the person has a total income less than a certain amount, you may be able to claim the person as a dependent.
Check with your tax adviser about these possibilities.
§
Mr. A Begins to Fall; It's PSP, Not Parkinson's

The first time he fell, he was raking leaves on their sloping front yard, and he fell over backwards. The second time, he lost his balance on a stairway. The third time, he didn't see a rock on the path and stumbled. No broken bones, but Mr. A., 61 years old, had several bruises and a sore back. His wife made him go to the doctor to see what was wrong.
A specialist thought Mr. A's walk was stiff and awkward. A CT scan of the spine was normal, indicating no direct spinal cord disease, so the diagnosis became "Parkinson's Disease" (PD). A drug for PD helped the stiffness a little, but Mr. A kept falling. They got a second opinion.
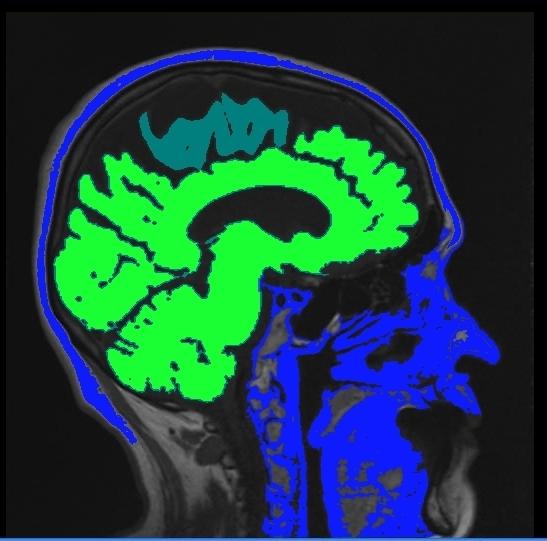
By this time, some other signs had appeared. His eyes did not move as briskly as they should. He especially had difficulty looking down. He became a sloppy eater, messing food off his plate. (It was hard for him to look down and see the plate.) He became compulsive in placing objects on the table. Sometimes he cried (it was not like him to cry), but returned to normal in a few minutes. These signs suggested an uncommon disease, Progressive Supranuclear Palsy (PSP). A brain MRI showed shrinkage of the top part of the midbrain (Figure), adding powerful credibility to the diagnosis of PSP.
What PSP Is
It's a progressive condition in which brain proteins alter their shape, called misfolding. No one knows how or why, but it is associated with alteration's of the protein tau, so it is one of the tauopathies.
How Is It Treated?
There is no cure, but some things can be helpful. To reduce falls risk, a walker is better than a cane. Since the patient tends to fall backwards, the walker should be weighted. Built up heels in the shoes also may help tilt the patient forward and reduce the risk of falling backwards. For more information, go to http://www.curepsp.org.
§
Best Blood Pressure Medication for Dementia?

ACE inhibitors are a group of blood pressure medications. They might be useful in treating dementia as well. In a Canadian study, over 300 subjects with dementia were followed. 85 were taking an ACE inhibitor. They did better than the others—they had slower decline—regardless of blood pressure.
ACE is an enzyme that produces angiotensin II, a powerful substance that squeezes arteries, limits blood flow, and requires the heart to push against a higher back pressure. ACE Inhibitor drugs block or limit ACE. This lets blood vessels relax, lowers the pressure and allows more blood to flow. In addition, ACE inhibitors increase bradykinin which also improves blood flow.
Reducing angiotensin II and increasing bradykinin may increase tissue blood flow and allow better tissue oxygen uptake. This might be useful in marathon runners and other athletes, as it may improve endurance.
Another reason to inhibit ACE: ACE may reduce acetylcholine, a critical neurochemical in the brain. Inhibiting ACE may lead to more acetylcholine, a desirable outcome in dementia.
Benefit in dementia was seen only with centrally acting ACE inhibitors. Available centrally acting ACE inhibitors include: ramipril, trandolapril, captopril, fosinopril, and lisinopril. One study showed perindopril outperformed other ACE inhibitors. Perindopril seems to be more lipophilic, meaning it may get into brain tissues more effectively.
Warning: ACE inhibitor drugs can have bad side effects, including cough, back pain, depression, edema, nausea, abnormal electrocardiogram, and elevated potassium. They may be dangerous if taken by some people.
Sources Gao 2013 Yamada 2011§
Now Whole Grain is Bad?

We should avoid gluten and whole grains, according to one specialist. Dr. David Perimutter asserts that gluten sensitivity is widespread, and not just in people diagnosed as gluten-sensitive. But what he talks about a lot is sugar, and glycemic index. And he's wrong, at least in one assertion. In an interview published by Medscape, a medical information news service, he said, "When you look at the glycemic index of whole-grain bread, for example, it's extremely high: 72-74. It's higher than that of white bread." However, according to a Harvard publication, whole wheat bread has the same or a lower glycemic index than white bread. Bread is made with sugar, and the amount may vary by the baker, so estimates are only approximate.
Glycemic index is probably important. It's a number that reflects how high blood sugar rises after eating a portion of the food. High blood sugar has been associated with higher risk of dementia. Whether this is due to a direct toxic effect of sugar, or an indirect effect from the insulin reflex is not known.
More important is the glycemic load. This is an estimate of how much one serving of food acts like pure glucose. Glucose causes insulin to rise, and sharp increases in insulin level are felt to be harmful. Dr. Perimutter uses drinking 2 glasses of orange juice a day as an example of carbohydrate overload. But his glasses of orange juice are 12 ounces, and two glasses would be 24 ounces. That's a lot of orange juice, and of course it's a lot of sugar. But the glycemic load of one six ounce glass of orange juice is less than the glycemic load of one slice of white bread. If you are concerned about insulin dynamics, consider glycemic load more than glycemic index.
Dr. Perimutter also says gluten can cause inflammation in the brain. Many foods can cause inflammation in the brain. It's not clear that it's a big problem, though. Animal fats can cause atherosclerosis, and many experts think that is the much more important problem. Many many nutritionists recommend a diet high in whole grains and low in animal fats.
Source: Grain Brain: The Surprising Truth About Wheat, Carbs, and Sugar -- Your Brain's Silent Killers, Dr. David Perlmutter,
Medscape Neurologyhttp://www.medscape.com/viewarticle/819232_2
§
.
Pamela is Attractive and Unlucky
By all accounts, Pamela is an attractive woman. Platinum blonde hair turning silvery gray, movie star face, pleasant smile, trim figure. Yet in spite of these to-die-for features, you would not want to be in her place.
Fifty eight years old, her husband died four years ago. When Pamela’s grief had begun to ebb, and she contemplated re-joining a more normal life, her widowed father was diagnosed with Alzheimer’s disease. Pamela sold her house to escape the haunting memories and moved in with her mother.
She didn’t understand the care burden she was getting into. She would have tried anyway, but she may have been more prepared if she understood. Caregiving is much more difficult than she ever expected. Her usually sweet dad denies that he has any problem, and gets angry, very angry, when Pamela tries to help him. Her father does not pay his bills on time, and buys into scams aimed at older people. Her father doesn’t take his medicines regularly, so his high blood pressure is not controlled. Often he does not take his thyroid medication for days—then takes it twice daily for more days, leading to a hormonal roller coaster of mood swings and energy. He wants to go places he shouldn’t, he cooks dangerously, his personal hygiene has slipped, and he generally “gets into trouble.” Pamela must be with her father all the time. “All…the…time,” she says, slowly. “The only time I am by myself is when I’m in the bathroom.”
Children aren't available to help Pamela. Her brother declined to help, “Too busy,” he said. Her mother would not tolerate an in-home aide. "I don't need one, and I won't have one," she declared. Pam has no control over her father's spending or other decisions except to nag and plead. Pam feels totally helpless and can see nothing in her future except being drawn into a caregiver's downward spiral of conflict and misery. Pamela is emotionally exhausted, physically tired, and spiritually drained. She suffers every day.
Lessons for Us?
Alzheimer's disease is increasingly prevalent. Almost all of us will have a family member with it in our lifetime. Are there lessons for us from this true story? "Should have/could have" advice is always easy after the fact, but this case does suggest some actions that could have been taken.
If her father had created a Durable Power of Attorney before she developed Alzheimer’s, Pam would have the authority to manage his finances, and make plans about household help. If Pam had learned about what to expect, and went to a dementia support group, she would be more mentally prepared. If Pam were not so benevolent and reticent, if she accepted the role of being the loving but determined "parent" to her father, rather than the child, she would set boundaries for her father's actions. She could demand help from her brother and his adult children. All these things will happen in time, except the Power of Attorney (Pamela will have to go to court and get Guardianship). The sooner these things happen, the sooner Pam’s life will begin to recover and move towards more normal, which she certainly deserves.
§
I Don't Think It Went Over Well
I gave a talk recently. It took hours to prepare. I talked about what I was supposed to, Alzheimer's disease. My presentation was lively. The visuals were informative and interesting. But I don't think it went over well.
The audience was intelligent, well educated people, experts in their fields, but with little healthcare background. My talk was the kind I give to students and doctors. It included an honest assessment of what is available to prevent and treat Alzheimer's disease. I explained evidence scales, in which research results are graded on their quality, which means how much you can trust the findings and implications for daily life. There is not much that can be done to prevent Alzheimer's, and there is nothing that stops or even slows its progress. Bummer!
I think the audience wanted to cling to myths they liked, and didn't like my honest scientific appraisal.
§
Myths People Want to Believe
- "If you treat mild memory impairment, you can prevent it turning into Alzheimer's." Sadly, that's just not true
- "If you treat Alzheimer's early, you can slow it down." No evidence to support that.
- "If you keep your brain busy, you won't get dementia." Insufficient evidence for that.
- "If you eat a lot of curry [or other pet supplement], you will never get Alzheimer's." Definitely not proven.
Lesson Learned
Next time, maybe I will just present my unproven but likable recommendations.
- - - - - -
My New (unproven) Recommendations to Reduce Your Risk of Alzheimer's
I. Take care of your heart and blood vessels. (Don't smoke. Keep your blood pressure under control. Keep your cholesterol low. Have regular physical activity.)
II. Have plenty of nighttime sleep, usually 8 hours for most people.
III. Avoid or reduce stress, or learn to be comfortable with stress.
IV. Eat a healthy diet.
V. Keep your brain active doing things you like to do.
Five Steps to a Healthy Brain...Almost Guaranteed!
§